Introduction:
In the realm of respiratory care, ventilators play a crucial role in supporting patients with compromised lung function. However, before these life-saving devices are utilized for patient care, it is essential to follow proper guidelines to ensure their optimal functioning and safety. In this article, we will explore the importance of ventilator pre-use checks and provide a step-by-step guide based on industry recommendations based on A White Paper from the American Association for Respiratory Care (AARC) and University
HealthSystem Consortium’s (UHC) Respiratory Care Network
Why Conduct Ventilator Pre-Use Checks?
Ventilator pre-use checks are a critical aspect of patient safety and quality care. These checks help identify potential issues or malfunctions in the equipment, preventing adverse events during ventilation therapy. By adhering to pre-use check guidelines, respiratory care professionals can ensure that ventilators are functioning optimally, settings are appropriate for patients, alarms are functional, and monitoring devices are accurately connected.
Step-by-Step Guide to Ventilator Pre-Use Checks:
- Visual Inspection:
- Thoroughly examine the ventilator, inspecting the power cord, tubing, and connectors for any visible damage or defects.
- Check for cleanliness and ensure there are no contaminants or debris.
- Power Source and Calibration:
- Verify that the ventilator is connected to a reliable power source and confirm the battery backup, if applicable, is fully charged.
- Perform calibration checks to ensure the ventilator is properly calibrated and sensors are functioning correctly.
- Alarm System:
- Test the alarm system by simulating various alarm conditions to ensure audibility and visibility.
- Ensure that alarms activate appropriately and respond to different alarm settings.
- Ventilator Settings and Parameters:
- Verify and double-check ventilator settings and parameters for accuracy.
- Confirm appropriate settings for tidal volume, respiratory rate, FiO2, and other relevant parameters based on the intended patient population and therapy.
- Monitoring Devices:
- Ensure that monitoring devices, such as pulse oximeters and capnography equipment, are properly connected and functioning correctly.
- Check the accuracy of readings and confirm that monitoring values align with the patient’s condition.
- Operational Check:
- Initiate the ventilator in standby mode and assess its response to user commands.
- Ensure that the ventilator is responsive and functions appropriately during the operational check.
Which Tools are Needed for Ventilator Pre-Use Checks?
Ventilator pre-use checks require specific tools to ensure accurate assessments of the equipment’s functionality and settings. Let’s explore the essential tools used during these checks:
- Visual Inspection:
- Well-lit environment for a thorough examination of the ventilator.
- Power Source and Calibration:
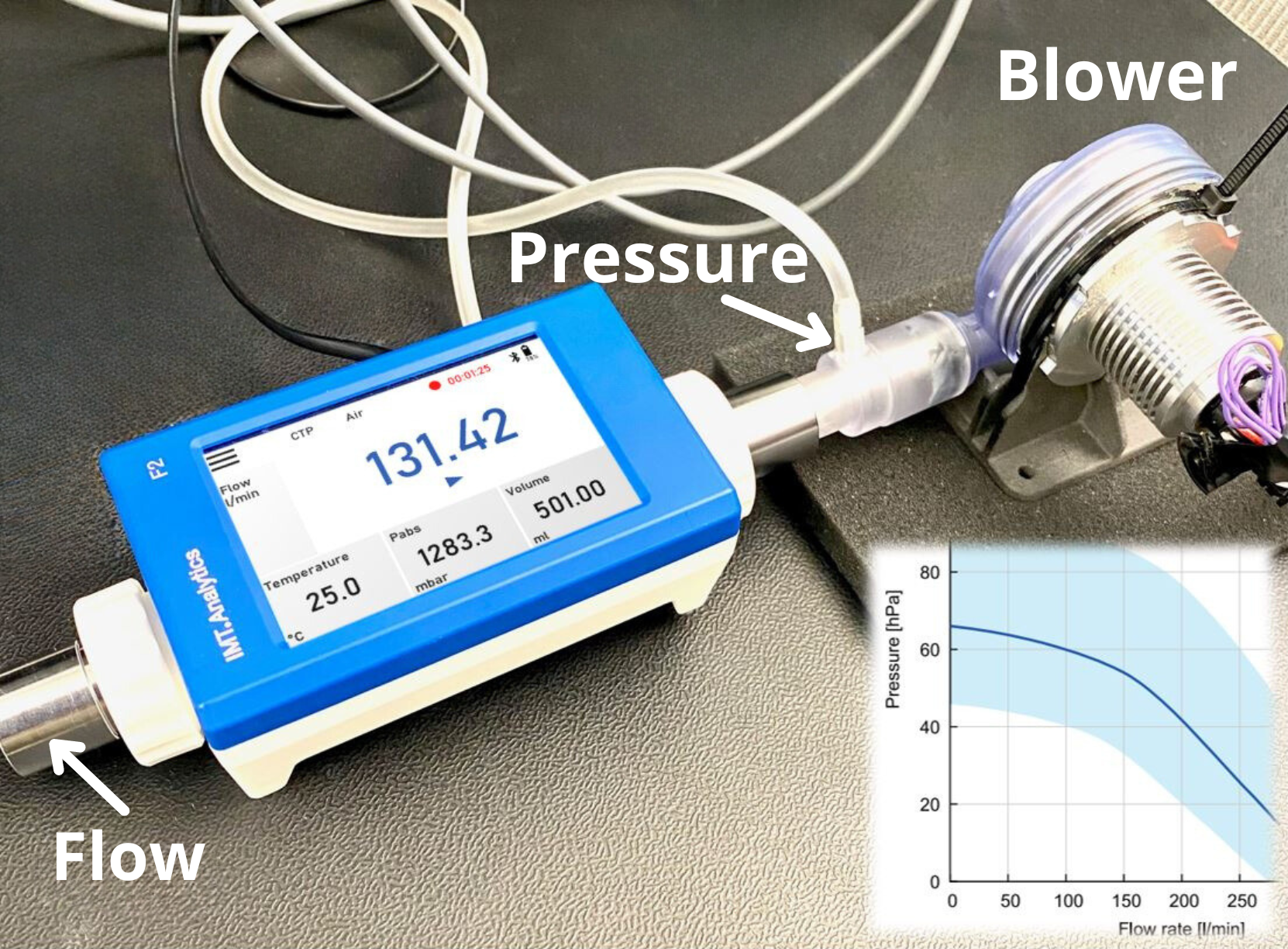
- Calibration tools (e.g., calibration syringe, pressure manometer or gas flow analyzer) may be required based on the ventilator model and manufacturer’s instructions.
- Alarm System:
- No additional tools are typically needed as the ventilator’s built-in alarm system is assessed by simulating alarm conditions.
- Ventilator Settings and Parameters:
- Access to the ventilator’s user interface or control panel is necessary.
- Gas flow analyzers: These instruments are used for accurate calibration of ventilator parameters such as tidal volume, respiratory rate, and inspiratory/expiratory time.
- Test lungs: They provide a simulated patient interface for evaluating ventilator performance and verifying appropriate settings.
It is important to emphasize the use of gas flow analyzers for calibration and parameter testing. Gas flow analyzers are independent measurement tools that offer precise and reliable readings. By employing gas flow analyzers, testers can ensure accurate calibration of the ventilator and verify proper ventilator settings. This independent measurement tool adds an extra layer of confidence in the accuracy of the ventilator’s parameters.
When performing Ventilator Settings and Parameters tests, it is recommended to rely on gas flow analyzers and test lungs to simulate patient conditions accurately. These tools enable thorough evaluations of the ventilator’s performance and ensure that the settings align with the specific needs of the patient.
By utilizing the appropriate tools, including gas flow analyzers and test lungs, healthcare professionals can conduct comprehensive pre-use checks on ventilators. These tools contribute to the accuracy, reliability, and safety of the ventilator’s operation, ultimately enhancing patient care and outcomes.
Who Performs Ventilator Pre-Use Checks?
Ventilator pre-use checks are typically performed by respiratory therapists, nurses or biomedical engineers specifically trained in respiratory care. These individuals have the necessary expertise and knowledge to conduct thorough assessments of the ventilator’s functionality and settings. They follow established protocols and guidelines to ensure patient safety and optimal ventilator performance.
It is important to note that specific healthcare facilities or organizations may have their own policies regarding who performs ventilator pre-use checks. However, it is typically within the scope of respiratory care professionals to conduct these assessments, given their specialized training and understanding of ventilator systems.
Conclusion:
Ventilator pre-use checks are an integral part of ensuring patient safety and quality care. By following the guidelines outlined in this article, respiratory care professionals can identify any potential issues with the ventilator before initiating therapy. Regular adherence to these guidelines minimizes the risk of malfunctions, enhances patient outcomes, and fosters a safer environment for ventilator-dependent patients.
Remember, it is crucial to consult the manufacturer’s instructions and guidelines specific to the ventilator model being used. By prioritizing proper pre-use checks, healthcare providers can provide optimal care and contribute to improved patient outcomes in respiratory therapy.